The vial on the lab bench looked like nothing special—just a thumbnail of clear liquid catching the cold fluorescent light. But if you leaned closer, past the hum of incubators and the soft clink of glassware, you’d notice the quiet gravity in the room. The researchers around it weren’t just measuring molecules. They were trying to pull monsters out of the dark.
Cancer has always been a disease of shadows. It hides in our own cells, slipping past the immune system like a master of disguise. For decades, treatments have tried to burn, poison, or cut it away. Powerful, yes. Brutal, often. But what if we could simply make cancer visible—so glaringly obvious that the immune system couldn’t help but see it, surround it, and tear it apart?
That is exactly what a new wave of research is attempting to do: teaching our own bodies to spot what’s been hiding in plain sight.
The Body’s Blind Spot
Imagine walking through a dense forest at dusk. The air is cool, filled with the damp smell of moss and earth. You can hear things moving—wings in the canopy, tiny feet in the underbrush—but you can’t see them. They’re there, but they blend so perfectly into the fading light that your eyes don’t register their shapes.
That’s how the immune system often experiences cancer. Our defenses are built to recognize what’s “foreign”—invading bacteria, viruses, parasites. Cancer is something more unsettling: our own cells gone rogue. Their DNA is scrambled, their behavior is reckless, but at their core, they still wear the uniforms of “self.” To many immune cells patrolling the bloodstream, they look like regular citizens, not traitors.
Under the microscope, it’s almost tragic. T cells—those sharp-eyed sentinels of immunity—drift past cancer cells without pausing. Macrophages, the body’s scavengers, nibble at dead material nearby but miss the thriving tumor a few microns away. The enemy is not just silent; it’s camouflaged.
This is why some of the most important cancer treatments of the last decade have focused on checkpoint inhibitors—drugs that remove the brakes from the immune system, giving it permission to attack. But even a fearless immune system has a problem if it can’t see what to attack.
Lighting Up the Invisible
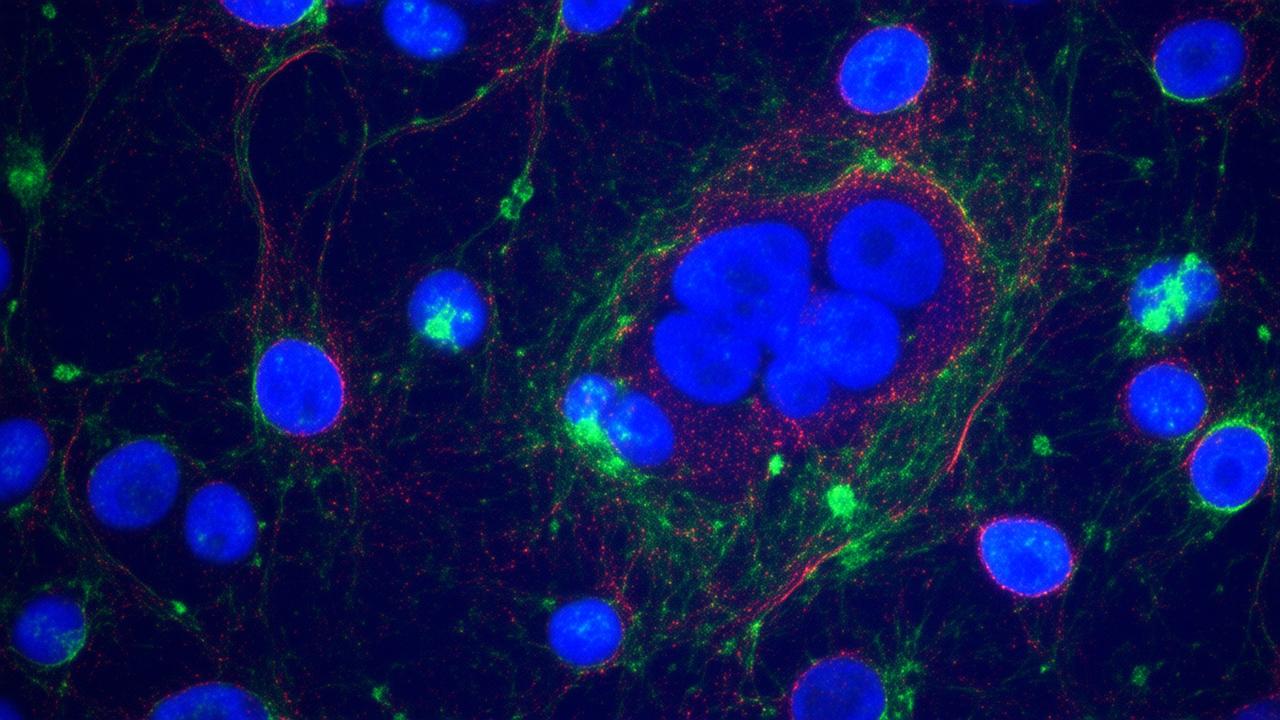
In one lab, late at night, a researcher glanced at a series of glowing images on a computer screen and felt something close to awe. Under the right dye, in the right conditions, the cancer cells were no longer ghostly outlines. They were lit up—a constellation of points shimmering with unmistakable clarity.
That image captures the heart of this new strategy: make cancer so visible that the immune system can no longer ignore it.
Scientists are developing ways to do this that feel almost like science fiction. One approach involves molecules that latch onto specific markers on cancer cells and essentially hang a bright “flag” on them. Another uses engineered proteins that force cancer cells to display distress signals on their surfaces—signals that immune cells instinctively recognize as: this doesn’t belong here.
Some of these strategies work like a biological highlighter pen:
- They find cancer-specific molecules on the cell surface.
- They bind tightly, forming a new layer of recognizable “tags.”
- Immune cells see these tags and swarm, like birds zeroing in on a berry-laden tree.
Others operate from the inside. They slip into the cancer cell, tweak how it communicates, and coax it into revealing pieces of its mutant proteins on the outside—almost like forcing a spy to wear a bright red coat in the middle of a crowd.
However it’s done, the goal is the same: erase the cancer’s invisibility cloak.
When the Immune System Finally Sees
To understand how powerful visibility can be, picture a coastal village with a fog-shrouded bay. Boats drift in and out, sometimes crashing on hidden rocks. Then one day, the villagers build a lighthouse. The rocks haven’t moved. The sea hasn’t calmed. But suddenly, danger has a shape—and that changes everything.
In the body, those rocks are tumor cells. The lighthouse is a new set of signals—bright molecular beacons that call immune cells in like search beams.
Once cancer cells are marked, something remarkable happens:
- T cells begin to recognize them as intruders, locking on with their receptors and delivering lethal hits.
- Natural killer cells join the attack, especially on cells that look “suspicious” or abnormal on their surface.
- Dendritic cells grab fragments of dying tumor cells and carry them deeper into the immune system’s training grounds, where new waves of cancer-specific T cells are educated and released.
It’s not just a one-time skirmish. The immune system starts to remember. Like a village that’s mapped every dangerous reef and shoreline, the body becomes better equipped to spot and attack similar cancer cells if they dare return.
In early experimental models, this visibility strategy has turned quiet, stubborn tumors into inflamed battlegrounds, where previously indifferent immune cells suddenly swarm with purpose. In some cases, tumors that resisted conventional therapies began to shrink when their invisibility was stripped away.
How Scientists Are Tagging Tumors
In the lab, the air often smells faintly of ethanol and agar, and the world narrows to petri dishes and pixelated images. But beneath the precise pipetting and sterile routines, there’s something almost poetic happening: scientists are trying to teach the body a new language of recognition.
They’re exploring several cutting-edge methods to make cancer cells stand out:
| Strategy | How It Makes Cancer Visible | Potential Benefit |
|---|---|---|
| Surface Tagging Molecules | Attach bright, recognizable markers to proteins on cancer cell surfaces. | Helps T cells and antibodies lock onto tumor cells more efficiently. |
| Engineered “Eat Me” Signals | Force cancer cells to display signals that attract immune cell attack. | Overrides cancer’s usual “don’t eat me” camouflage. |
| Neoantigen Amplifiers | Enhance the presentation of mutant cancer proteins on cell surfaces. | Makes each tumor cell more uniquely identifiable as abnormal. |
| Immune-Guiding Nanoparticles | Deliver tags or stimulants directly into the tumor’s neighborhood. | Focuses the immune response where it is needed most. |
| Imaging + Therapy Hybrids | Use imaging tracers that also act as immune-visible markers. | Lets doctors see and treat tumors with the same targeting system. |
What makes this so groundbreaking is not only what these strategies do, but where they fit. They can sit alongside existing treatments: surgery, radiation, chemotherapy, and immunotherapies like checkpoint inhibitors and CAR-T cells. Visibility becomes the missing link—helping all these tools find clearer targets.
In some experimental setups, for example, tagging tumors first and then using checkpoint inhibitors appears to supercharge outcomes. It’s like giving a search team not just permission to act, but a detailed map of exactly where to go.
The Human Stories Behind the Science
Behind every lab breakthrough are people who have waited in dim hospital rooms, counting the drip of IV bags and the beeps of heart monitors. This isn’t just molecular choreography—it’s a possible shift in how future patients might experience cancer treatment.
Imagine a patient walking into a clinic not to be told, “We’re going to carpet-bomb your body with chemicals,” but instead: “We’re going to help your immune system see what it’s been missing.”
That doesn’t mean it will be easy. Even the most elegant therapies come with side effects. When the immune system wakes up strongly, it can misfire, sometimes attacking healthy tissues in its zeal. Researchers must find the narrow path between powerful and safe.
Still, there’s something deeply intuitive—and deeply hopeful—about this direction. Instead of relying only on external, often harsh treatments, we’re learning how to support the body’s own defense storytelling: teaching it who the villain is, how to find it, and how to remember it.
➡️ A quieter housing revolution is unfolding through passive cooling design and smarter shading systems
➡️ New long COVID clinics are reshaping how chronic illness is diagnosed and managed
➡️ Desalination plants are becoming central to water security plans despite energy concerns
➡️ New shark tracking data is changing safety planning at popular swimming beaches
➡️ A revival of handwritten learning is gaining momentum in schools wary of screen overload
➡️ Wildlife carers are warning of a tougher year as habitat loss meets extreme weather
➡️ A new generation of museum curators is revisiting repatriation and colonial collecting ethics
In one trial, a patient with a tumor that simply would not respond to standard drugs was given a therapy designed to unmask the cancer cells. Weeks later, scans showed new, bright areas of immune activity around the tumor: hot, inflamed, full of fighting cells. It wasn’t a magic cure. But it was a conversation begun between body and disease—a conversation that had never fully happened before.
What This Could Mean for the Future
If you zoom out from the petri dishes and clinical scans, this strategy hints at a quieter revolution: a world in which cancer care is less about brute force and more about intelligent visibility.
The promise is not just more powerful treatments, but potentially:
- Earlier detection: If tumors can be tagged at smaller sizes, we might find them before they become deeply entrenched.
- More personalized medicine: Each person’s cancer has its own unique set of abnormal proteins; visibility tools can be tailored to those specific fingerprints.
- Long-term immune memory: By engaging the immune system deeply, visible tumors could lead to better protection against recurrence.
There will be challenges. Tumors are clever, constantly evolving. Some may change their surface markers to escape new tags. Others may burrow deeper into tissues where immune access is limited. And the complexity of the immune system means no single solution will fit every patient, every cancer type, every stage.
But the idea—turning the lights on—has taken hold. It’s not about making cancer simpler; it’s about making it less able to hide.
Somewhere in a hospital imaging suite, a physician might one day look at a scan where a tumor glows not just as a shape in the organ, but as a living, targeted structure the immune system is already circling. In that moment, the old sense of helplessness might loosen its grip just a bit.
A New Kind of Light in the Dark
Back in the lab, the vial of clear liquid is returned gently to its stand. It’s easy, in that fluorescent quiet, to see only the glass and the numbers. But there’s another way to see it: as a small lighthouse in a long, foggy night.
Cancer has always thrived in obscurity, borrowing our own identity to evade notice. Now, science is beginning to answer with a different kind of power—not just stronger weapons, but sharper sight.
As these visibility strategies move from experimental models into clinical trials and, eventually, into standard care, they carry with them a subtle but profound shift in philosophy: that perhaps the most radical thing we can do is to help the body see what’s been there all along.
In the end, this story is not only about molecules or markers. It’s about the ancient pact between a body and its defenders, renewed. A quiet agreement: if you show me the danger, I will do everything I can to protect you.
Frequently Asked Questions
Is this visibility strategy a cure for cancer?
Not yet. It’s a powerful new approach that could significantly improve how well existing treatments work, especially immunotherapies. But cancer is complex, and most patients will still need a combination of therapies. The visibility strategy is best understood as a major new tool, not a single, universal cure.
How is this different from current immunotherapy?
Many current immunotherapies focus on boosting or unleashing the immune system. This new strategy focuses on helping the immune system see cancer cells more clearly. When combined, visibility and activation could make immune-based treatments much more precise and effective.
Will this work for all types of cancer?
Researchers are hopeful, but it’s unlikely that any one method will work equally well for every cancer. Different tumors express different markers and behave differently in the body. Scientists are developing varied tagging and unmasking techniques to match different cancer types.
Are there risks to making cancer cells more visible?
The main risk is that a highly activated immune system might also target healthy tissues, leading to inflammation or autoimmune-like side effects. Clinical trials are designed to carefully monitor and manage these reactions, balancing power with safety.
When might patients start to benefit from these approaches?
Some early-stage clinical trials are already underway, but it can take years for new therapies to move through testing, approval, and widespread use. However, the underlying ideas are already influencing how researchers design the next generation of cancer treatments, so their impact is beginning now and will likely grow over the coming decade.